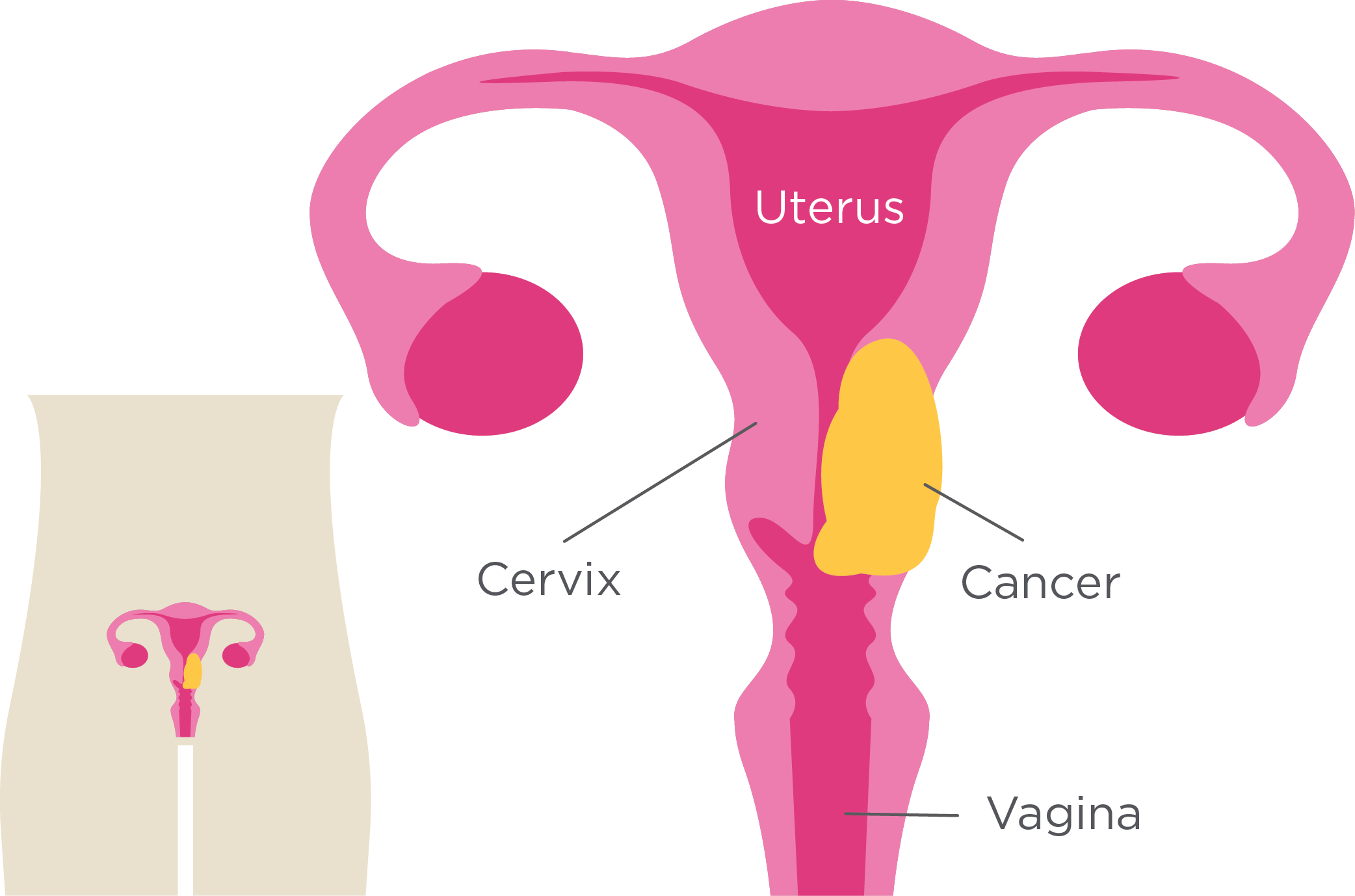
What is Cervical Cancer?
Cervical cancer is a type of cancer that starts in the cervix, the hollow, tunnel-like organ connecting the lower end of the uterus (womb) to the vagina. It is among the most common cancers that aect Malaysian women.
The vast majority of cervical cancers are caused by certain types of human papillomavirus (HPV). HPV is a common infection that is spread through sexual contact. Over time, HPV might develop into cervical cancer. That is why screening is vital to detect HPV and cervical cancer in the early stages so that it can be effectively treated.
What are the Symptoms of Cervical Cancer?
- Unusual vaginal bleeding (after intercourse, between periods, or after menopause)
- Pelvic pain or pain during intercourse
- Unusual vaginal discharge (watery, bloody, or foul-smelling)
- Painful urination or blood in urine
- Diffculty urination
Other symptoms include:
- Back or leg pain: As cancer progresses, it can cause pain in the lower back or legs
- Weight loss: Unintended weight loss can be a sign of advanced cervical cancer
- Fatigue: Persistent tiredness that does not improve with rest


Cervical Cancer Screening
The most reliable method of detecting cervical cancer is pap smears and HPV tests. The symptoms of cervical cancer are sometimes mistaken for other less serious health conditions, so it is best to incorporate cervical cancer screening into your health check-ups. Both pap smears and HPV tests involve collecting cell samples from the vagina with a small brush or spatula. While similar in terms of their methods, the dierence between the two tests is that a pap smear detects precancerous or cancerous cells, whereas an HPV test detects the presence of human papillomavirus.
Screening Guidelines
Depending on your age and health history, the frequency of testing may vary.
| Age Group | Screening Recommendations* |
|---|---|
| Below 30 years old | Screening is recommended if sexually active |
| 30 - 65 years old |
Initial screening: Yearly pap smear for the first two years.
If initial results are normal: Standalone pap smear every 3 years or pap smear and HPV co-testing every 5 years. Alternatively, standalone HPV testing every 5 years |
| Above 65 years old | Screening may be discontinued if you had regular screenings with normal results. Consult your doctor for personalised advice. |
*Women with a history of cervical cancer, exposure to DES before birth, HIV infection, organ transplant or who have a weakened immune system may need more frequent screening.
What Happens During Cervical Cancer Screening
During a pap smear or HPV test, you will need to undress from the waist down, lie on an exam table with your feet in stirrups, and the doctor will gently insert a speculum into your vagina to look at your cervix. They will then use a small brush or spatula to collect cells from your cervix, which might cause a little pressure or discomfort but should not hurt.
Once the speculum is removed, you can get dressed. The whole process takes just a few minutes. You will be informed when the results are ready, usually between a few days to a week
How Do I Prepare for Cervical Screening?
Before the test
Schedule the test to happen on a day when you are not on your period. Inform the doctor or medical staff:
|
|
If you had any abnormal pap smears/HPV tests or cervical issues in the past |
|
|
Mention any medications or health conditions you have |
For 2 days before the test, avoid:
|
|
Sexual intercourse |
|
|
Using tampons |
|
|
Douching (cleaning the inside of your vagina) |
|
|
Using vaginal creams or medications |
During the test
|
|
Wear comfortable clothes that are easy to take off |
|
|
Practise deep breathing to stay calm |
After the test
|
|
You might experience light spotting or mild cramping, but there should not be any serious complications.If you experience discomfort that lasts more than a few minutes or bleeding for more than 24 hours, contact the hospital. |
|
|
If your results appear abnormal, it does not necessarily mean you have cancer. Your doctor will discuss the results with you and determine the next course of action. |

How to Reduce the Risk of Cervical Cancer?
As the single biggest risk factor for cervical cancer is HPV, the best ways to reduce the risk of developing cervical cancer include:
-
HPV vaccination
-
Limit the number of sexual partners
-
Use protection during sexual intercourse
-
Regular STD screenings
Like with most cancers, it is best to quit smoking and maintain a healthy lifestyle to reduce the risk of cancer